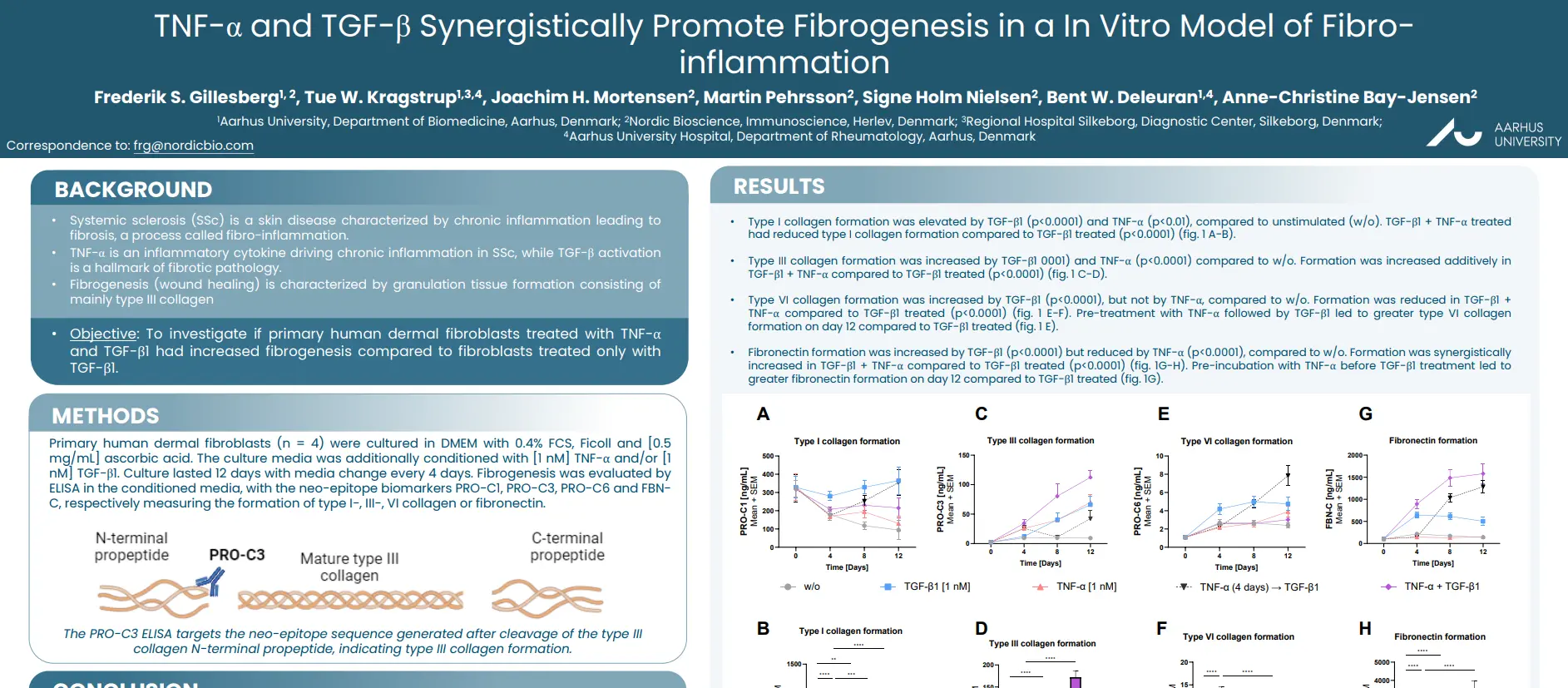
TNF-α and TGF-β Synergistically Promote Fibrogenesis in a In Vitro Model of Fibro-inflammation
Introduction
Systemic sclerosis (SSc) is a skin disease characterized by chronic inflammation leading to
fibrosis, a process called fibro-inflammation. TNF-α is an inflammatory cytokine driving chronic inflammation in SSc, while TGF-β activation is a hallmark of fibrotic pathology. Fibrogenesis (wound healing) is characterized by granulation tissue formation consisting of mainly type III collagen.
The aim of this study was to investigate if primary human dermal fibroblasts treated with TNF-α
and TGF-β1 had increased fibrogenesis compared to fibroblasts treated only with TGF-β1.
Poster
Conclusion
Inflammatory TNF-α stimulation increases TGF-β driven fibrogenesis in dermal fibroblasts, by promoting their formation of type III collagen and fibronectin. Consequently, biomarkers of type III collagen formation and fibronectin formation may be markers of early fibrosis in fibro-inflammatory skin disease.