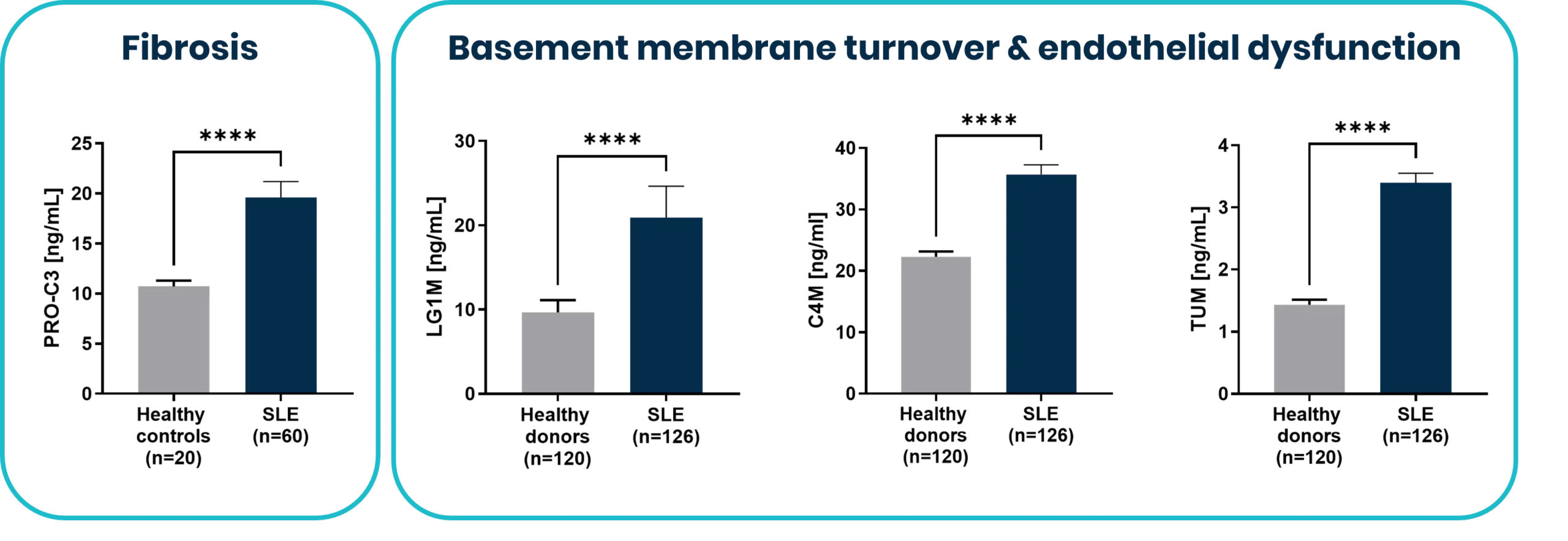
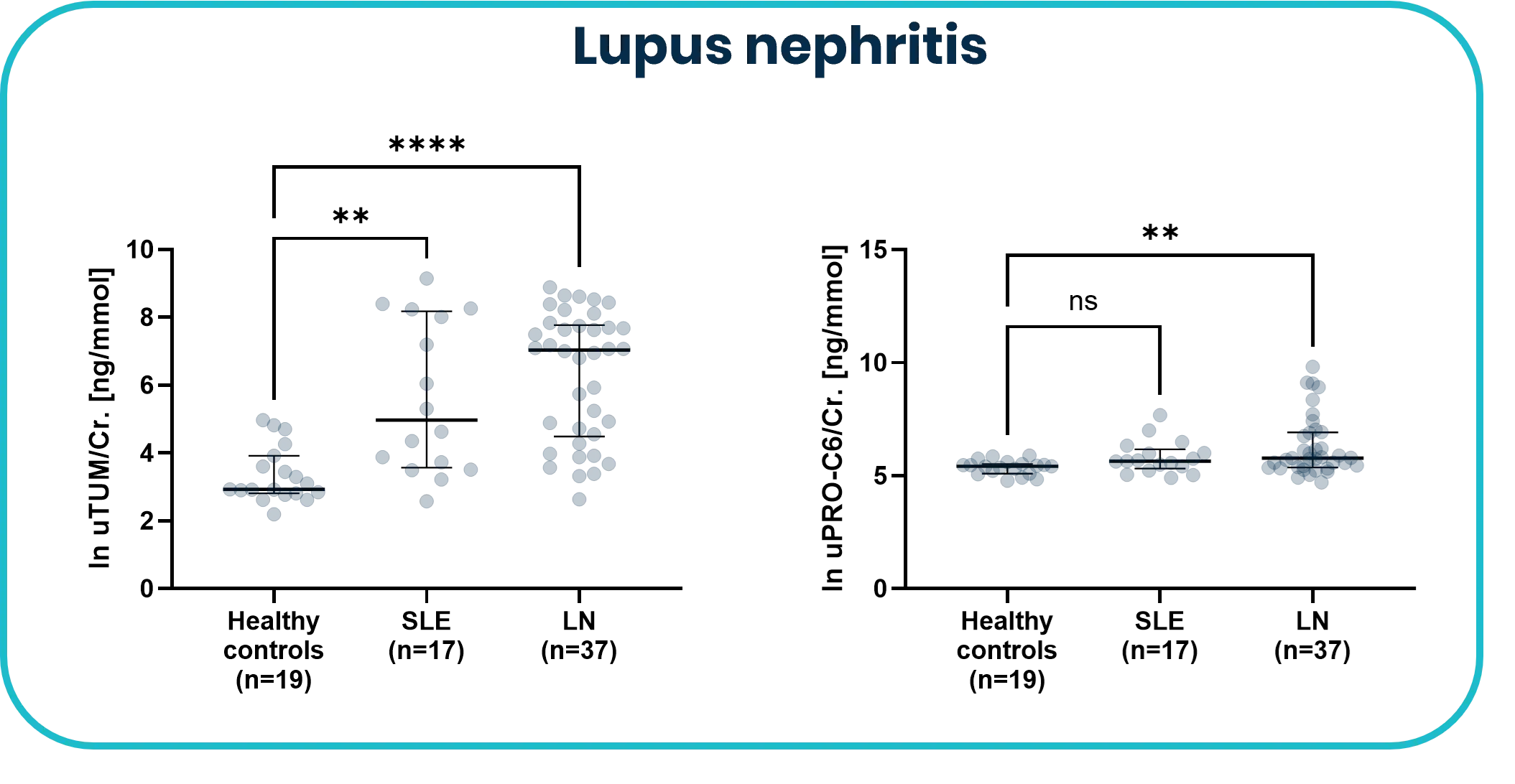
Systemic lupus erythematosus (SLE) is a complex and heterogeneous autoimmune disease marked by episodic flares, multi-organ involvement, and progressive tissue damage driven by both immune activation and impaired resolution. Despite advances in serological testing, conventional biomarkers often fail to reflect the dynamic tissue-level changes occurring during disease progression.
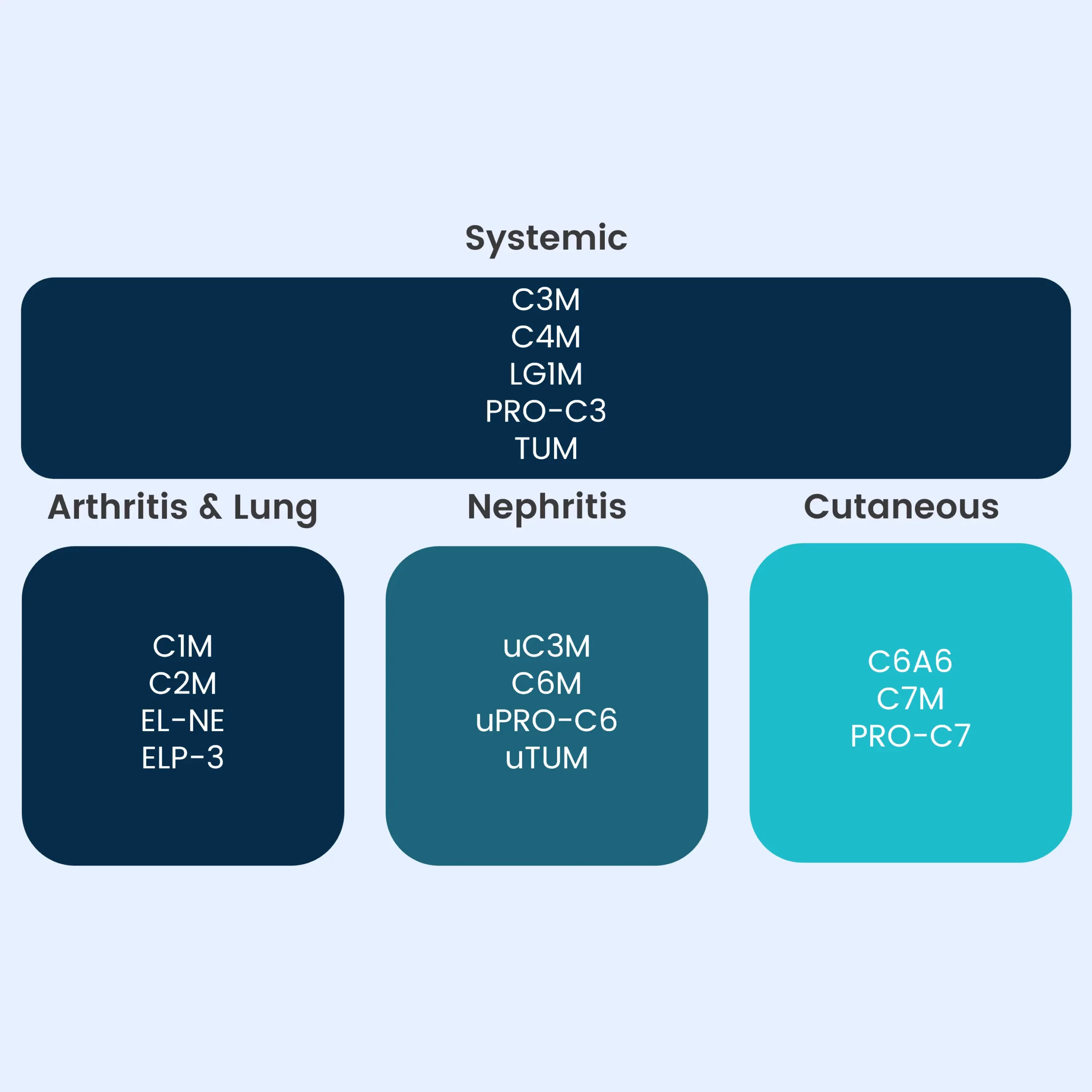
Moreover, they offer limited ability to distinguish between distinct organ-specific manifestations, making treatment decisions and response monitoring challenging in clinical practice.There is a growing need for biomarkers that can capture disease activity at the tissue level, support endotyping, and enable precision medicine approaches in SLE.