Chronic respiratory disease is a collective term for diseases affecting the airways and other structures of the lungs. These diseases are major contributors to global mortality and the overall burden on health. Some of the most common types are chronic obstructive pulmonary disease (COPD), asthma, and pulmonary hypertension, diseases which all exhibits various subtypes.
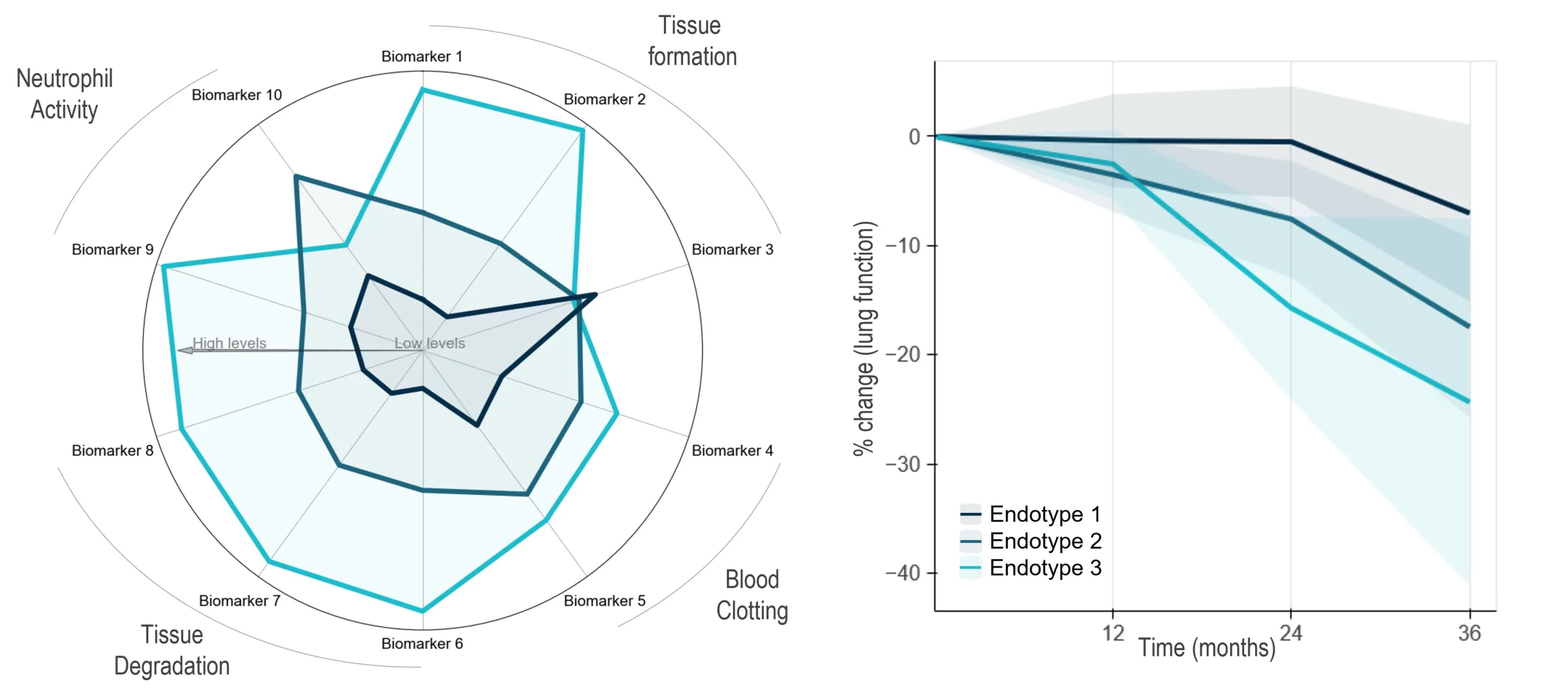
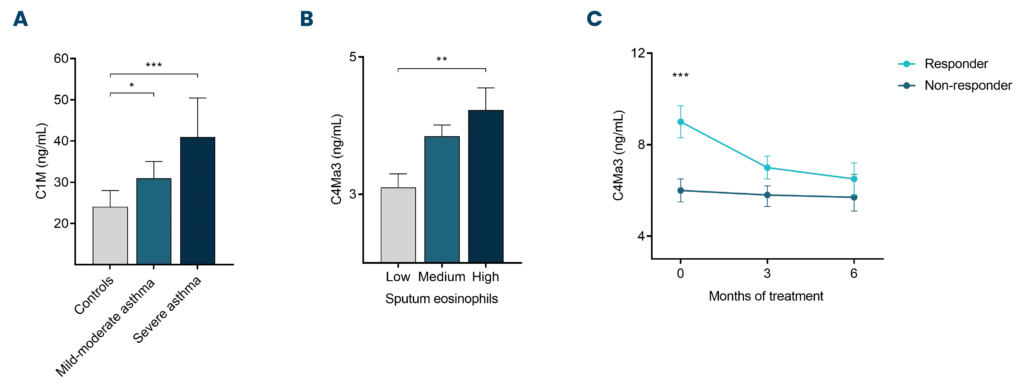
Characteristics of these diseases are the changes to the lung tissue and the inflammatory microenvironment, leading to both lung tissue destruction and the deposition of excess proteins in the wrong location.
Did you know?
Nordic Bioscience develops non-invasive blood-based biomarkers which can be used as tools to quantify these key pathological changes in the lung. These biomarkers can help us understand the complex molecular pathways that lead to chronic respiratory disease and promote personalized treatment options.