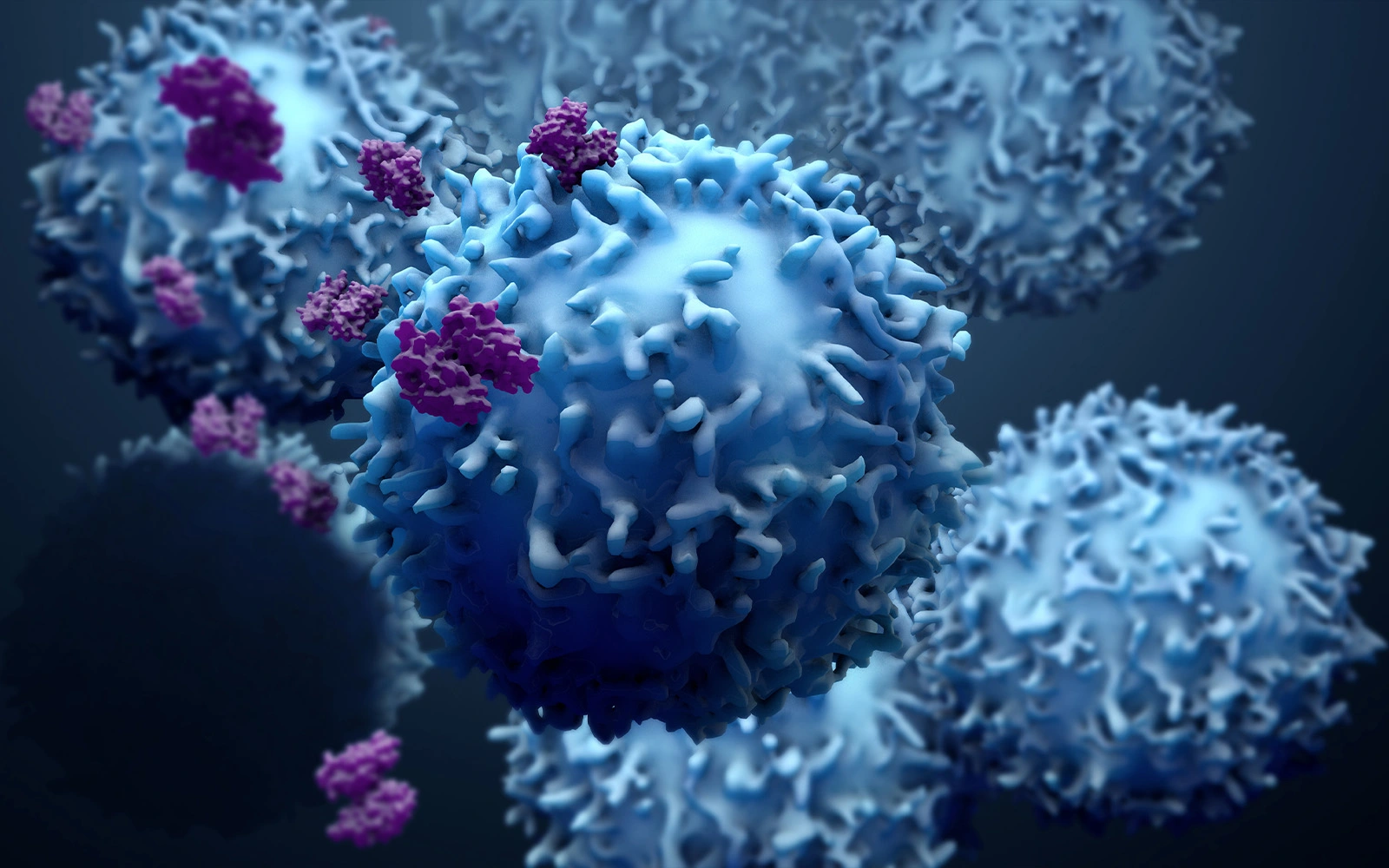
The field of immuno-oncology is based on decades of research into how tumors have acquired mechanisms to circumvent and evade elimination by the immune system. By intervening with the ability of tumors to escape the immune system and by re-activating and re-directing immune cells in the tumor microenvironment, immuno-oncology therapies enable the body’s own defense system to recognize and eliminate the tumor.
One essential characteristic of patients benefitting from immuno-oncology therapies such as checkpoint inhibitors is that their T-cells are present and/or recruited to the tumor. That is, if T-cells are not homing to the tumor, treatment will have a poor effect. Therefore, it is important to identify patients with a T-cell permissive tumor microenvironment.
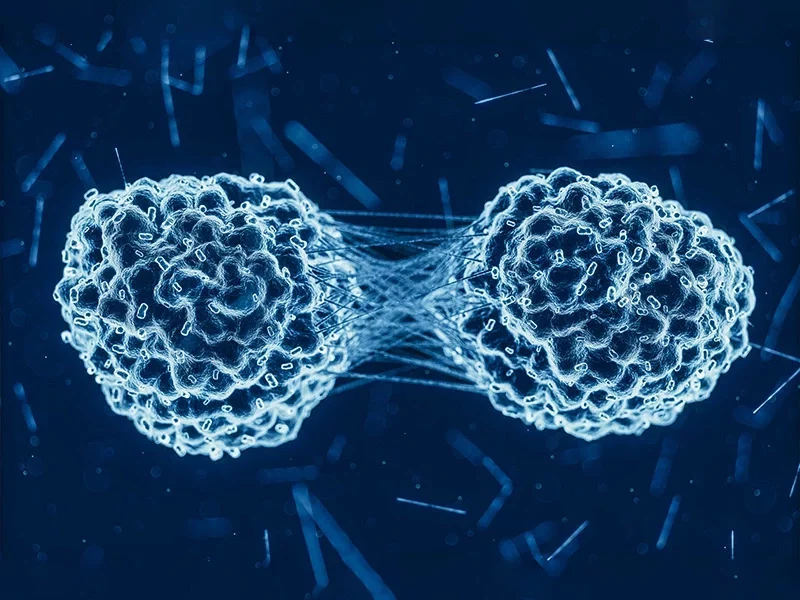
Analysis of the tumor microenvironment in patients with a variety of solid tumors has revealed that patients can be divided into phenotypes based on T-cell infiltration: tumors with T-cell infiltration (“hot tumors”/”inflamed tumors”) and tumors without T-cell infiltration (“cold tumors”/”excluded tumors”).
Interestingly, it has been shown that T-cells are actively degrading the basement membrane extracellular matrix when transmigrating from the blood and into the tumor, and the architecture of the extracellular matrix defines the localization and migration of T-cells within the tumor with T-cells being entrapped in the dense interstitial extracellular matrix and therefore cannot reach and kill the tumor cells.