Lupus nephritis (LN) is a serious manifestation of systemic lupus erythematosus and a leading cause of kidney damage in affected patients. Despite immunosuppressive therapies, many patients experience ongoing renal injury that leads to fibrosis and progressive loss of kidney function.
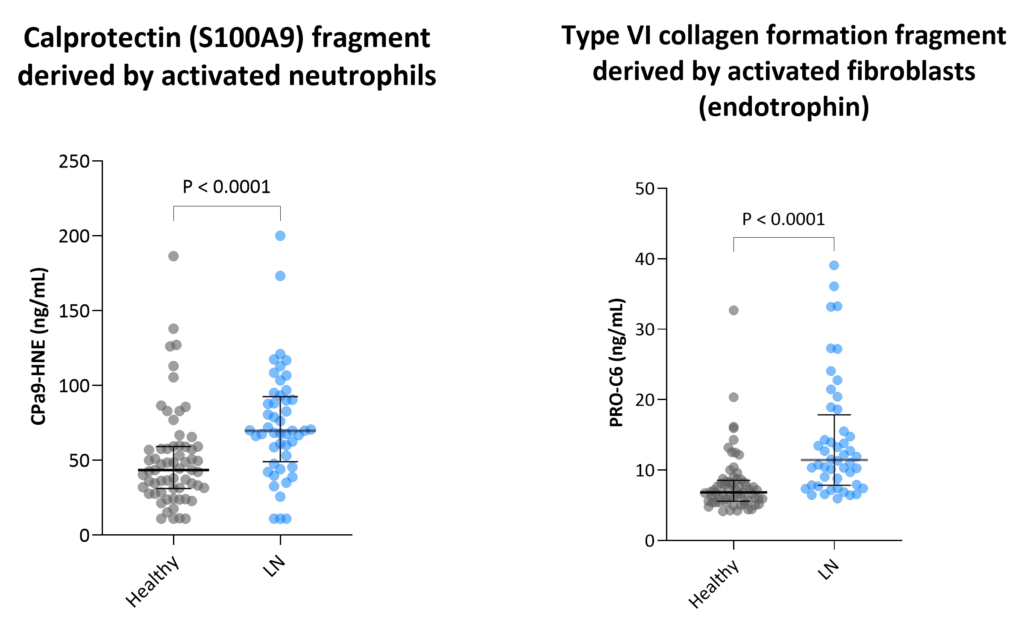
Traditional clinical markers such as proteinuria and serum creatinine often fail to detect early fibrotic changes or capture dynamic treatment responses. This highlights the need for more sensitive and mechanistic biomarkers that can provide deeper insight into underlying disease processes, particularly tissue remodeling. In LN, extracellular matrix (ECM) accumulation and turnover are central to the development of chronic kidney scarring. ECM-derived biomarkers can offer a direct, non-invasive, and biologically relevant assessment of disease activity by capturing ongoing fibrogenesis and fibrolysis.